A recent study published in BMC Health Services Research examines how access to community-based behavioral healthcare services influences the per capita jail population. Here, we summarize the background, purpose, design, and findings of the research. The full, original article, entitled "The relationship between community public health, behavioral health service accessibility, and mass incarceration," is available here.
Background
Of the 10.3 million people incarcerated in U.S. jails in 2019, 45% reported a history of mental health issues. Those held in jails have been shown to meet the criteria for "serious psychological distress" at levels five times higher than the general population, "with nearly half reporting serious psychological distress in the past 30 days."
Although the U.S. has an incarceration rate three times higher than comparable countries, very little research has been conducted to determine "the interplay between the size of jail populations and community-level behavioral health services."
Purpose
"The goal of the current study is to bridge the gap in the literature to explore factors related to behavioral health services in the community, as well as the demographics and socio-economic factors, that may predict jail utilization."
According to the authors: "This study examines how socio-economic, health, behavioral health, and justice factors are related to per capita jail population in U.S. counties."
This purpose is tied to several factors:
- As of 2014, 10 times more people with serious mental illness were being held in jails or prisons versus psychiatric hospitals run by the state.
- Treatment for those with a history of mental illness or displaying serious psychological distress is provided for less than half of those in jails.
- Structural factors, such as bail laws and changes in housing or employment, lead to more people with mental illness being incarcerated.
- "Community capacity to treat behavioral health disorders is extremely low;" however, "incarceration may detrimentally impact the physical and behavioral health of a community. Recent estimates indicate that as increases occur in jail incarceration rate, increases also occur in county-wide mortality from substance use and suicide, as well as a range of diseases and injuries."
- Those living in rural communities have access to fewer providers of mental healthcare, as well as outpatient facilities—and Medicaid is less likely to be accepted.
- Communities with a higher low-income population, as well as those with higher Black and Hispanic populations, have reduced access to behavioral healthcare. This impacts those in need of care to address substance use issues and mental health needs.
- "Limited community mental health services restrict the options communities have to respond to individuals with behavioral health disorders who commit crimes."
Design
The authors examined data from 3,141 counties in the U.S. collected between 2014 and 2019. Sources were as follows:
- Incarceration trends were examined using data from the Vera Institute.
- Health, economic, social, and demographic information came from the Robert Wood Johnson Foundation's County Health Rankings & Roadmaps (CHRR), which is compiled by the University of Wisconsin.
- The Uniform Crime Report was used to examine police data.
- The U.S. Census was used to determine per capita rates by county for behavioral healthcare services.
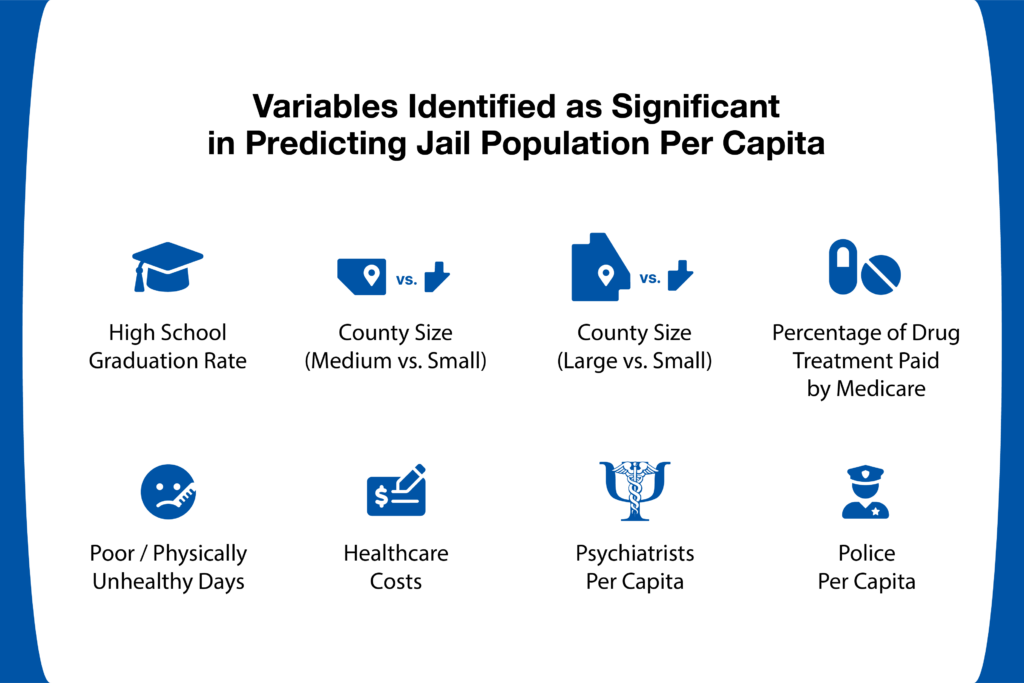
Data was reviewed by "a diverse panel of criminologists, psychologists, mental health professionals, biostatisticians, and health economists." Machine learning was then used to identify and select the 12 most important independent variables in determining predictors for per capita jail populations by county.
Findings
After conducting both a statistical analysis and beta regression, the study's authors found several key predictors of jail population and/or incarceration rates. For example:
- "More physically unhealthy days within the past 30 days predicted a higher per capita jail population."
- A lower level of behavioral healthcare capacity, higher costs for care, and fewer options for behavioral healthcare drug treatments covered by Medicare all related to a higher jail population, per capita.
- In fact,
"behavioral healthcare access and affordability factors were better predictors of per capita jail population than violent crime rate."
- The only justice system-related variable that predicted the presence of a larger jail population in a community was "a greater concentration of police"—yielding a 16% increase in those jailed for every additional officer.
- Small counties were found to have the highest jail population per capita. Medium counties' populations were approximately 15% fewer and large counties 40% fewer.
Conclusion
Based on the results of the studies, it's clear that communities with greater access to behavioral healthcare services that are affordable to residents "have significantly lower incarceration rates per county." Meanwhile, "smaller counties that are health resource-challenged, and those that are more policed, have larger per capita jail populations."
Investment and/or focus on improving mental health and behavioral healthcare services, including substance use treatment, may increase a community's ability "to use diversion and/or alternatives to incarceration to decrease the demand for jail beds." This is especially true for smaller counties that possess fewer resources, because "mental health and substance use care have been found to be more cost-effective at promoting recovery and reducing subsequent crime than incarceration."
* References available upon request.